Basic Life Support
Here i will share about basic life support. Recently basic life support/CPR class was held in chest hospital which attended by staff nurse,SDU and Nursing director. Class was brought by Dr Saad and Dr Khalid for 4 hour divided into 2 session, theory and practice.It was very interesting class,even though we already got this lecture when we were in the nursing college or even course in the hospital where we worked but still we need to learn more to make us more familiar,always remember and for refreshment of the new theory, as we know that knowledge is changing and improving
CPR IN ADULT
I would like to specify CPR in adult only.
There are 5 step that we usse to call DR ABC;
1.Danger
Before starting to help other we must check whether there is danger around ,for example fire, knife , leaking gas. if its there we must anticipate so it won't harm not only the victim but also for us as rescuer.we want help other but wont hurt us
2.Response

To make sure whether someone is really unconsius, we can call his/her names,and shake the shoulder,if there is no response we haave to call for help, ambulance/777 if posible then we go to next step
3.Airway
Directly open the air way with two technique:
-Head tilt chin lift maneuver if sure there is no neck injury other wise
-Jaw trust maneuver
the purpose are to open the obstruction of the tongue.
we have to make sure also whether there is foreign body like food or anything with cross finger technique .
4.Breathing
LOOK,LISTEN and FEEL the present of breathing,if none give 2 rescue breathing.
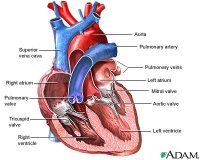
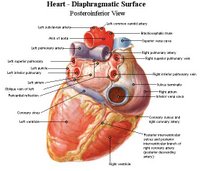
5.Circulation

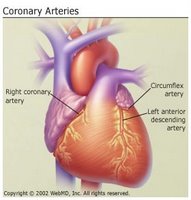
Check the presence of carotid pulse by putting two finger on the carotid vein site, if none then start CPR by compressing the heart,to put the heel of one hand interlock with another hand, on the sternum just two finger above the xiphoid.
-for one rescuer give 2 breathing then 30 compression
-for two rescuer continuous compression with breathing every 4-6 second
(this is the latest one, as we know before 1 rescuer is 2 breath 15 compression, 2 rescuer 2 breath 5 compression).

When we have to stop CPR?
1.Patient gain breathing and circulation
2.Ambulance/medical team arrived
3.Rescuer is very tired, can't continue CPR
4.Patient died
*)pictures taken from http://depts.washington.edu
Read more!